Article / Publication
Source: The Journal of Clinical Endocrinology & Metabolism
Key Takeaway: Nationwide reimbursement of real-time CGM improved HbA1c, fear of hypoglycemia, and QOL as well as economic indicators including work absenteeism and hospital admissions for acute diabetes complications.
The Value of rtCGM: Reduction in Hospitalizations and Work Absenteeism
| Pre-Reimbursement for rtCGM | Post-Reimbursement for rtCGM | P Value | |
| (n = 496) | (n = 379) | ||
| Patients with | |||
| Hospitalizations due to hypoglycemia and/or ketoacidosis | 77 (16%) | 14 (4%) | <0.0005 |
| Hospitalizations due to hypoglycemia | 59 (11%) | 12 (3%) | <0.0005 |
| Hospitalizations due to ketoacidosis | 23 (5%) | 4 (1%) | 0.092 |
| Work absenteesim* | 123 (25%) | 36 (9%) | <0.0005 |
| Days (per 100 patient years) of | |||
| Hospitalizations due to hypoglycemia and/or ketoacidosis | 53.5 | 17.8 | <0.0005 |
| Hospitalizations due to hypoglycemia | 38.5 | 12.5 | 0.001 |
| Hospitalizations due to ketoacidosis | 14.9 | 5.3 | 0.220 |
| Work absenteeism | 494.5 | 233.8 | 0.001 |
Data are n (%).
*Work absenteeism of at least half a day. Patient-reported hospital admissions were validated by clinicians.
Reference: Charleer S, et al. Clin Endocrinol Metab. 2018;103(3):1224–1232
 |  |
 |
Reference: Charleer S, Mathieu C, Nobels F, et al. J Clin Endocrinol Metab. 2018;103(3):1224-1232.
LEARN MORESource: Journal of the American Medical Association
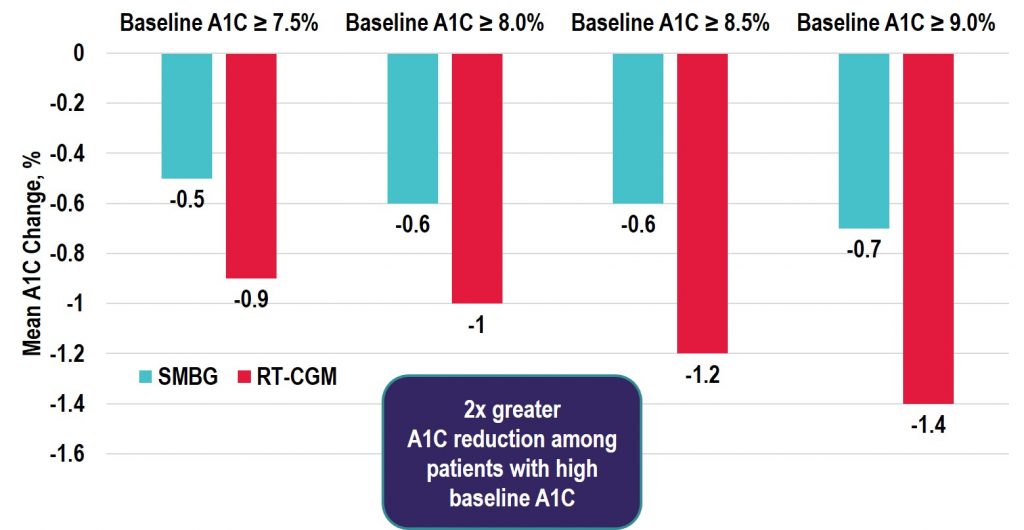
Key Takeaway: In the DIAMOND RCT, patients using multiple daily injections of insulin with type 1 diabetes who were randomly assigned to real-time CGM (rtCGM) had improved glycemic control vs. the SMBG group. This benefit was seen across patient groups regardless of baseline A1C, age, education level, or math ability. In addition, the rtCGM group spent 79% less time in nocturnal hypoglycemia, and also demonstrated a greater increase in hypoglycemic confidence and a greater decrease in diabetes distress vs. the SMBG group.
Learn MoreSource: Diabetes Technology & Therapeutics
Key Takeaway: Among the real-time CGM (rtCGM) users, the change in HbA1c was greatest in the highest HbA1c subgroup with similar decreases seen in both the T1D and T2D groups. Notably, adherence remained high in those with baseline HbA1c > 9% and the improvements seen were achieved without the need for additional medications. Thus, the costs of rtCGM in patients with high HbA1c may be offset by avoiding treatment intensification and the longer-term savings achieved by lowering HbA1c levels in poorly controlled diabetes populations.
Source: Journal of the American Medical Association
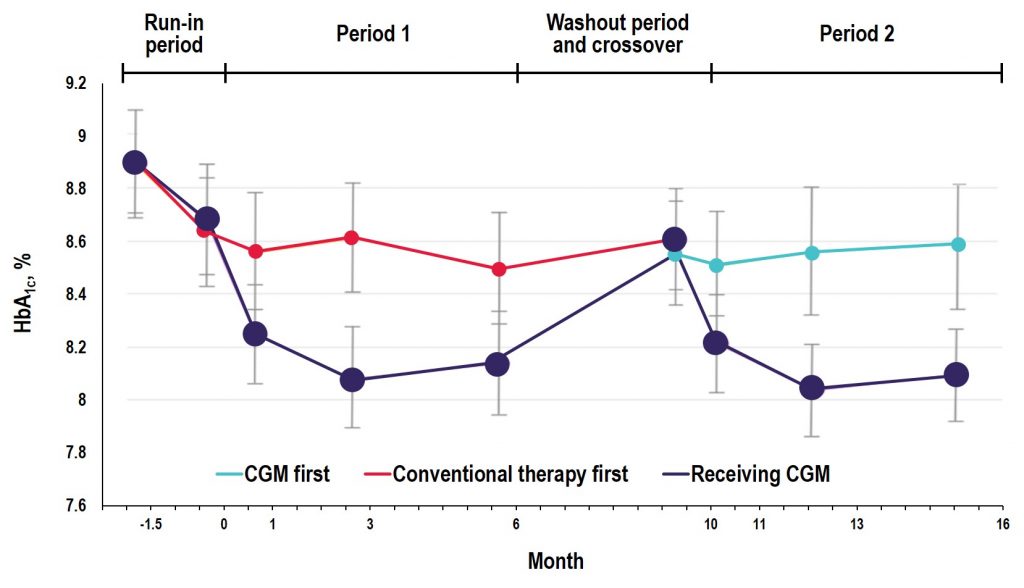
Key Takeaway: In the GOLD trial, glycemic control was improved with use of rtCGM compared with conventional treatment; however, increases in A1C and hypoglycemic events occurred when patients reverted back to SMBG during the crossover/washout period, suggesting that the effectiveness of CGM depends on uninterrupted use during treatment with MDI. Additionally, the study showed reductions in severe and nocturnal hypoglycemia as well as in glycemic variability and improved hypoglycemic confidence for rtCGM users.
Source: Diabetes Care
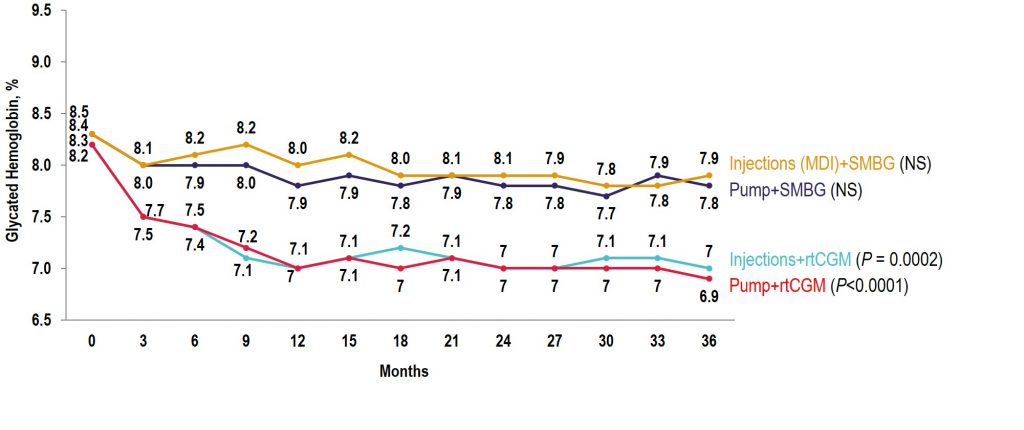
Key Takeaway: The COMISAIR study is the longest running real-world real-time CGM (rtCGM) study performed to date. In this study, the continuous use of rtCGM had a sustained and durable benefit with regards to glycemic control over a 3-year time period, with rtCGM being superior to self-monitoring of blood glucose in reducing A1C, hypoglycemia, and glycemic variability in individuals with type 1 diabetes regardless of their insulin delivery method.
Observational COMISAIR Study in Patients With T1D Who Chose Insulin Delivery Method (MDI or Pump) and Monitoring Method (SMBG or CGM), Staying on Chosen Therapy for 3 Years
Source: The New England Journal of Medicine
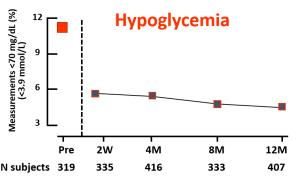
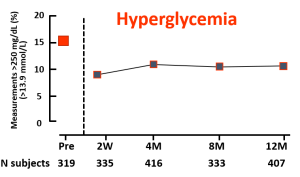
Key Takeaway: This 6 month randomized trial showed use of a closed-loop system using the t:slim X2 insulin pump with Control-IQ Technology, (Tandem Diabetes Care) and a continuous glucose monitor (Dexcom G6, Dexcom) was safe and effective compared to sensor-augmented pump therapy (SAP). Participants in the closed-loop group achieved 70% time in range overall which meets the International Consensus Guidelines for people with diabetes. The closed-loop group also achieved significant improvements in hyperglycemia, HbA1c, mean glucose, and hypoglycemia (< 70 mg/dL < 54 mg/dL) as compared with the SAP group. Glycemic benefits were seen in the first month of the trial and were sustained over the entire 6-month period. Over 90% of participants said they trusted the device and found Control-IQ technology easy to use.
*Full article available for a fee
Learn MoreSource: The Lancet
Key Takeaway: This study conducted in Europe with over 300 participants found novel flash glucose testing reduced the time adults with well controlled type 1 diabetes spent in hypoglycaemia. Future studies are needed to assess the effectiveness of this technology in patients with less well controlled diabetes and in younger age groups.
Learn MoreSource: Diabetes Care
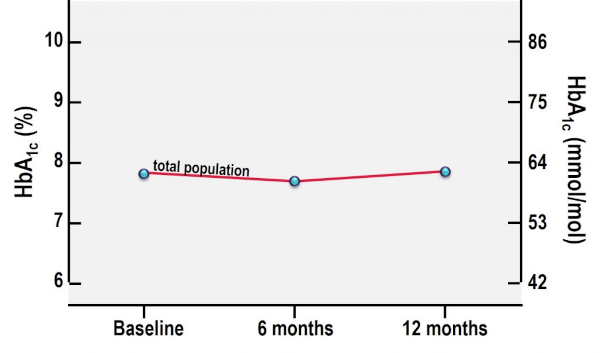
Key Takeaway: Nationwide unrestricted reimbursement of isCGM in people with type 1 diabetes treated in specialist diabetes centers results in higher treatment satisfaction, less severe hypoglycemia, and less work absenteeism, while maintaining quality of life and HbA1c.
A1C From Baseline to 12 Months After Initiation of isCGM
Source: American Association of Clinical Endocrinologists
Conclusion: CGM improves glycemic control, reduces hypoglycemia, and may reduce overall costs of diabetes management. Expanding CGM coverage and utilization is likely to improve the health outcomes of people with diabetes.
LEARN MORESource: The IQIVA Institute
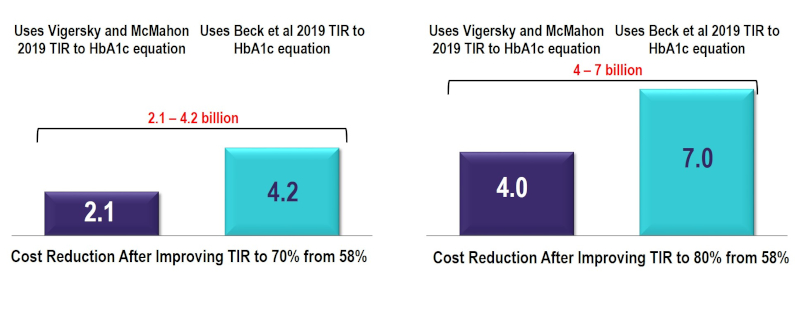
About the report: The incorporation of time in range (TIR) metrics alongside HbA1c is expected to enhance the way in which diabetes is managed in the future, and subsequently, reduce the overall societal and economic burden. To assess the value of improving TIR from its current state to the minimum consensus target of 70% and 80% TIR, the IQVIA Core Diabetes Model was used to estimate cost reductions in complications and costs associated with improving TIR. Using this model, improvements in TIR were estimated to reduce the risk of developing diabetes-related complications resulting in a conservative reduction of $2.1-7 billion in costs over a 10-year period, based on the relationship between TIR and HbA1c. The addition of incrementally reducing hypoglycemic events in people with Type 1 Diabetes by 40% and improving TIR to 80% generated a total 10-year cost reduction of $6.7-9.7 billion. This reduction in costs represents a conservative estimate.
10-Year Cost Reduction by Improving TIR in People with T1 and T2 Diabetes to 70% and 80% TIR (US$Bn)